PRP GROWTH FACTOR INJECTIONS
MAGNOVISION THERAPY
PHOTOBIOMODULATION THERAPY
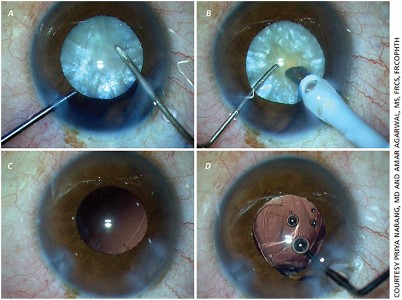
ARGUS II RETINAL PROSTHESIS OPERATION
The eyeball consists of refractive settings that focus light on the retina from front to back. The cornea is at the front and the lens behind it focuses the light on the retina.
The eyeball consists of 3 layers from the inside out. The innermost retina is the vascular layer in the middle, and the outermost is the white of the eye that gives the eyeball its rigidity.
Objects can be seen when the rays coming from the objects focus on the retina. There are cells in the retina that convert light energy into electrical energy and transmit it to the brain. These are called photoreceptors. Photoreceptors consist of two groups:
- Cone cells: images formed in the center and in a bright environment,
- Rod cells: processes images formed in the surrounding and dark environment.
In other words, they convert the rays coming from the objects into electrical energy.
Electron microscope view of the section taken from the retina. Just above the lowest pigment epithelium are photoreceptor cells consisting of rods and cones.
Retinitis pigmentosa begins with a mutation, or defect, in the genes of photoreceptor cells.
250 different genetic mutations lead to 50 different types of this disease. For this reason, clinical symptoms and progression rate are different in each patient. It is usually familial due to consanguineous marriage, but it can also occur non-familial.
Genetic mutation leads to premature aging and progressive death of photoreceptor cells. As age increases, cell death accelerates.
Growth factors enable the conversion of glucose in the blood to ATP-GTP, which is the cell fuel. In the absence of growth factors, photoreceptor cells slow down their metabolic activities due to energy deprivation, go into sleep mode, and if the process continues, cell death occurs progressively.
The growth factors that keep the photoreceptors alive are not secreted by the pigment epithelium and Müller cells, which show stem cell characteristics. Photoreceptors go into sleep mode for a long time before slowly dying. At this stage, the cells are alive but do not participate in the function of vision.
Which cells go into sleep mode or die first, symptoms begin accordingly. For example, if the rod cells start to die first, the first symptom will be reduced night vision.
In some genetic types of the disease, cone cells are affected before rod cells are affected. The cone cells first go into sleep mode and then die.
This condition is seen in stargarth disease, reverse rp, or cone dystrophy.
Here, the first symptom is excessive glare in the light, and better vision in dim environments and at night. As the disease progresses, central vision is lost and peripheral vision is preserved.
Retinitis Pigmentosa Treatment:
1) Stem Cell and Gene Therapy :
Its studies are still in progress and the target group is the patient group who has not completely lost their sight and has living cells in sleep mode. The rationale of stem cell therapy is to inject cells capable of secreting growth factor between 6 months and 2 years, into or around the eye, and repeat this process every 6 months or 2 years.
In gene therapy, the faulty gene in photoreceptors that have not lost their vitality is detected, the corrected gene is loaded into viruses and injected into the eye. The aim is again to stop the death of living photoreceptors.
2) Early diagnosis:
The earlier the diagnosis is made, the death of the remaining cells may be slowed down as much as possible without further loss of photoreceptors, may be stopped, or even cells in sleep mode may be awakened.
3) Growth factor injections
Ngf, bdnf, bfgf, IL6 are growth factors necessary for photoreceptors to maintain their vitality and functions.
First loading and then re-injection at certain intervals may slow down or stop the course of the disease. In some cases, depending on the presence or number of cells in sleep mode, visual field enlargement and visual acuity may be increased.
Enlargement of the visual field after the 3rd injection
4) Okuvision & Magnovision
Electromagnetic stimulation of the retina and the visual center in the brain not only increases the secretion of the necessary growth factors in the nervous system, but also allows the formation of new visual pathways called neuronal plasticity and the reorganization of visual function.
The awakening of the photoreceptors in the sleep mode and the enlargement of the visual field in the patient who underwent growth factor injection together with magnovision are shown in the figure below.
5) Treatment of complications
Cataract develops frequently in rp patients. In advanced stages, retinal vessels become thinner and oxygen reaching the intraocular tissues and essential nutrients decrease. This accelerates the development of cataracts.
Cataract operation in rp patients can accelerate cell death in the retina and cause excessive increase in macular edema. For this reason, protecting the retina with growth factors before cataract operation will minimize the possible risks.
Macular edema is another common complication in rp patients. Edema at a certain level does not require treatment as it meets the growth factor requirement for photoreceptors. However, edema that impairs visual acuity and becomes cystoid requires treatment. If it cannot be controlled with eye drops, edema should be controlled with intraocular injections.
6) Safety glasses
Filtering blue-violet light at a wavelength of 415-455 nm reduces the photoreceptor death rate by 25%. It is especially recommended for computer users.
500 nm orange lenses are recommended for rp patients with initial cataract or excessive glare in the light where cone cells are also affected.
7) Low vision rehabilitation tools:
In patients whose cone cells are affected and peripheral vision is good, telescopic glasses, magnifiers with light, or magnifiers with CCTV cameras respond particularly well to the reading needs of the patients.
8) Intraocular telescopic lens implantation:
Prismatic telescopic intraocular lenses, which shift the image out of the dead area, give satisfactory results in suitable patients in patients whose cone cells are affected and peripheral vision is good.
9) Nutrition-healthy life:
It is possible to slow down the death rate of photoreceptors by consuming foods high in antioxidant vitamins and minerals and food supplements. B12-b6-b1-folic acid and omega-3 are especially necessary for the vital activities of neuronal cells, while vitamin a-lutein-carotene is necessary for the synthesis of pigments necessary for the visual function of photoreceptors.
Mediterranean Type Nutrition
- Grilled Salmon: 2 days a week (all fatty fish – on the condition that they are grilled or baked)-(fried fish has no benefits.)
- Plenty of green salad + grated carrots
- Soft-boiled eggs: 3 days a week (boiled eggs in apricot consistency)
- Raisins with black seeds or fresh black grapes in season: once a week, handful
- Raw almonds: once a week, handful
- Walnut: once a week, handful
- Kefir: 2 days a week, 1 glass
30 minutes of walking outdoors every day
Absolutely no smoking
Abstinence from alcohol
It will greatly slow down the death rate of photoreceptors.
10) For patients whose photoreceptors have completely lost their vitality:
Virtual vision and rehabilitation with chips to perform the function of photoreceptors.
The image is perceived by a camera – converted into electrical energy and transmitted to the brain by electrodes. For this,
- brainport v200
- argus 2 bionic eyes
- cortical prosthesis
The most appropriate method is applied to the appropriate patient.